
We strive to share information about the fundamental importance of sanitary practices. That is why previous blog posts have endeavoured to convey the multitudinous benefits of preventing cross contamination. The term HAI has thus been used frequently and an overall picture has been sketched.
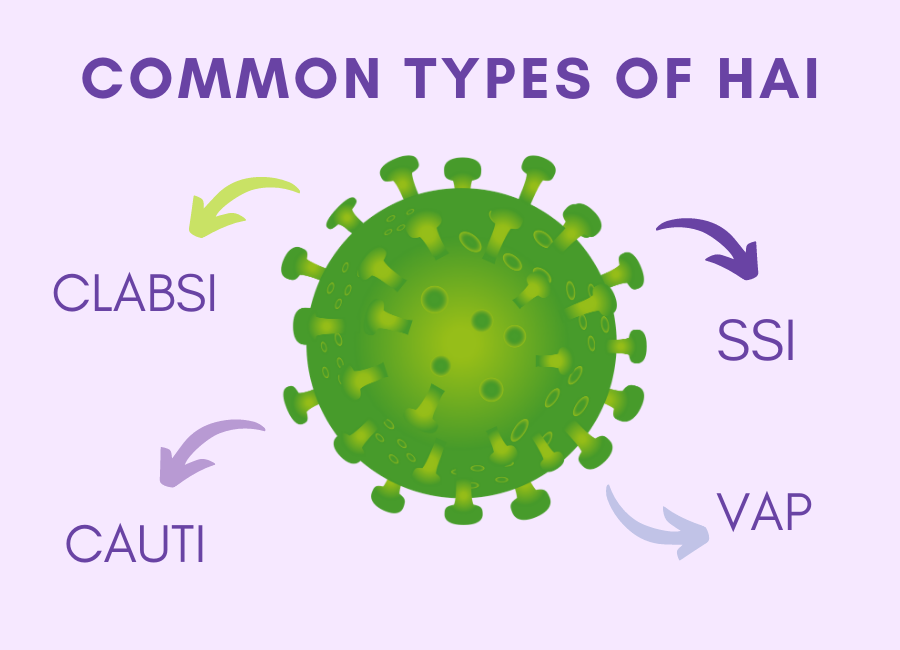
Comprehending the finer details of HAI allows us to understand how these infections infiltrate not only hospital settings but different parts of the body. A more detailed understanding of these infections can better inform our healthcare practices and perceptions.
There are 4 major/ common categories of HAI that have a pervasive and negative influence on the healthcare arena. The detailed profiles below, that have been compiled thanks to insights from the CDC, aim to provide vital information about each category.
This prolonged period of usage is where problems around sanitary practices usually arise.
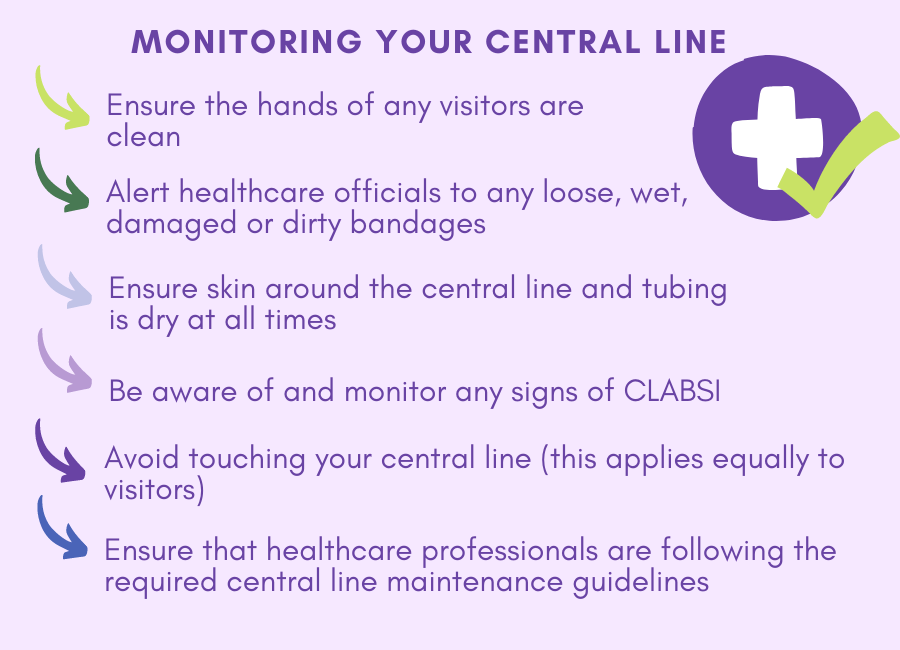
Germs enter the central line and pass through it into the patient’s bloodstream. As a result, the tube must always be inserted correctly and according to precise guidelines. Additionally, the site where the tube is inserted must be monitored and kept in pristine condition.
Signs that an infection has occurred are as follows: red or sore skin where the line has been inserted, as well as fever or chills. Medical tests will reveal if a CLABSI has set-in.
Both patients and healthcare workers alike can implement measures to maximize infection control.
The points below outline a few examples of precautions that can be implemented when a healthcare professional inserts a central line.
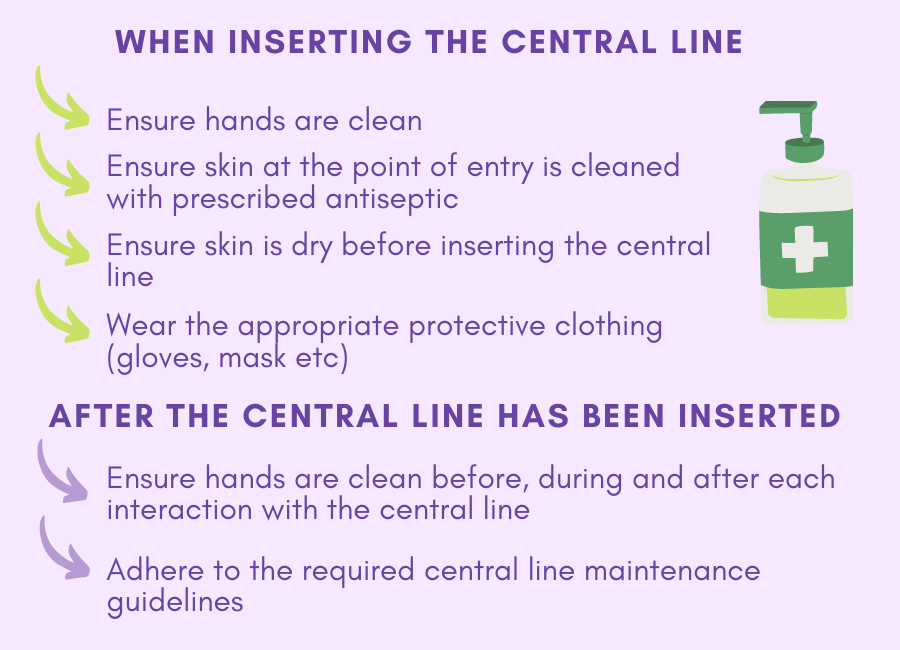
It is equally important to note that a central line must be removed as soon as it is no longer required.
Patient awareness is also important. The steps below will assist you in ensuring that optimal practices are followed.
If you are interested, click here to access a study done on instances of CLABSI in South African neonatal intensive care units.
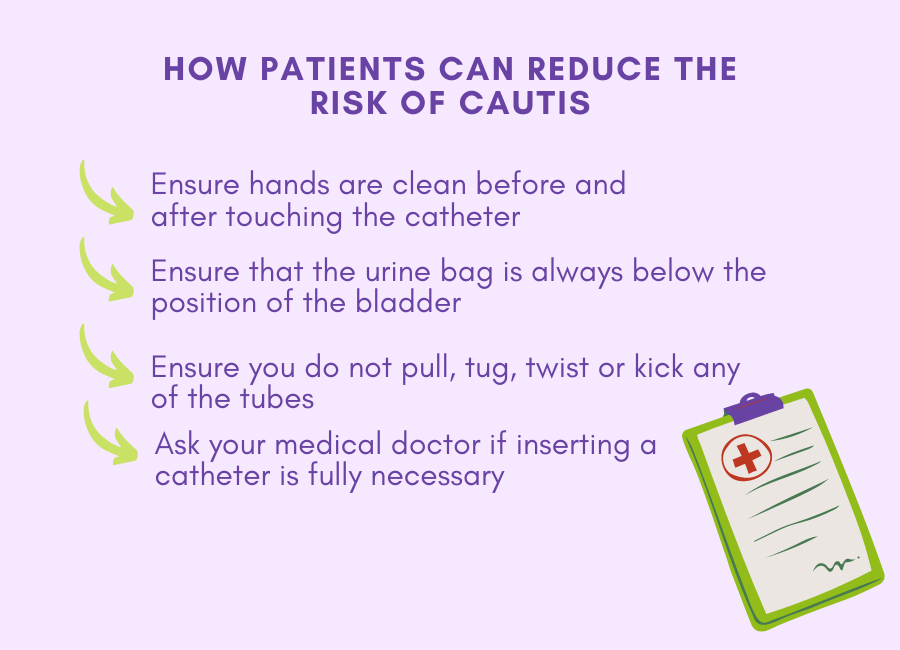
Germs enter the urinary tract, through the catheter and cause an infection. Whilst most infections can be cured with antibiotics or the use of a new catheter, CAUTIs are preventable if precautions are put in place.
Antiseptic and sanitary procedures must be maintained at all times, as this will reduce the possibility of germs contaminating the catheter. So too, the collection system must be monitored and maintained. As a result, there are different strategies that offer guidance to healthcare professionals.
Click here to access information with regards to the CDC’s:
Patients can be equally proactive and help prevent CAUTIs by implementing the following behaviour:
A SSI occurs when a patient goes in for a surgery and the site where the operation was performed becomes infected. This is usually indicated by a fever, pain or redness at the surgery site and if drainage fluid from the site is ‘cloudy’.
Depending on the nature of the surgery, a SSI can negatively affect anything from skin to tissue, implants and internal organs. Whilst SSIs can often be treated with antibiotics, often another surgery is required. This not only puts the patient at further risk but wastes valuable medical resources.
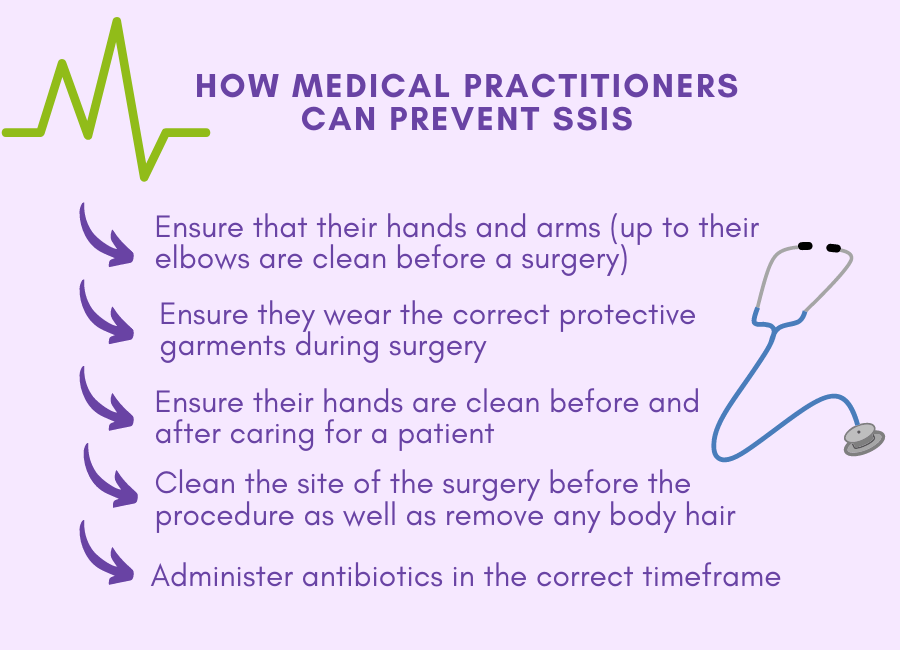
As with the above-mentioned HAIs, various methods can be implemented to reduce the risk of SSIs. The following details outline what healthcare practitioners should do to maintain infection control, specifically when their patients undergo a surgery.
If you are going for a surgery and would like information as to how you can reduce your risk of contracting an SSI, click here.
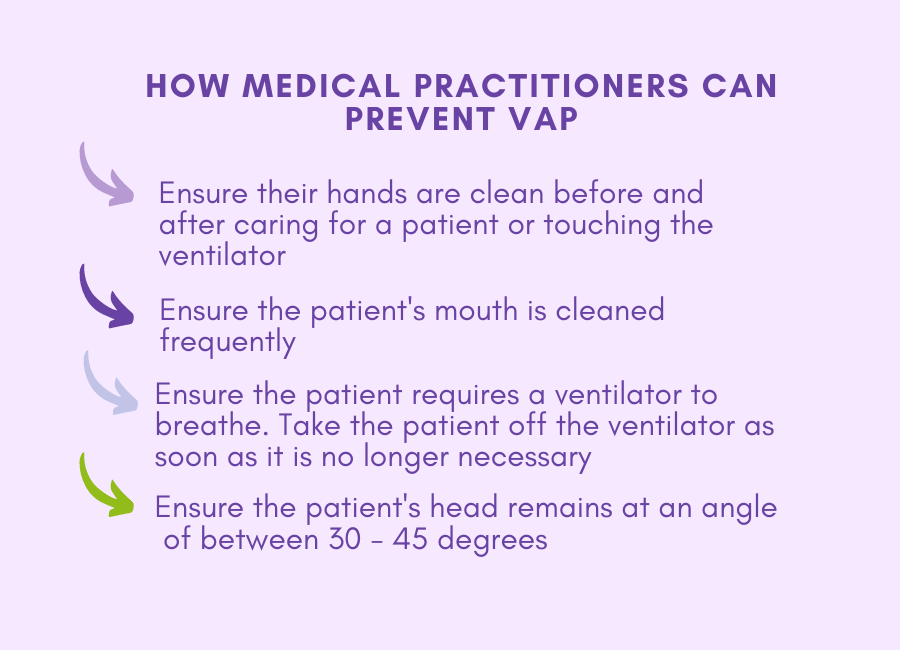
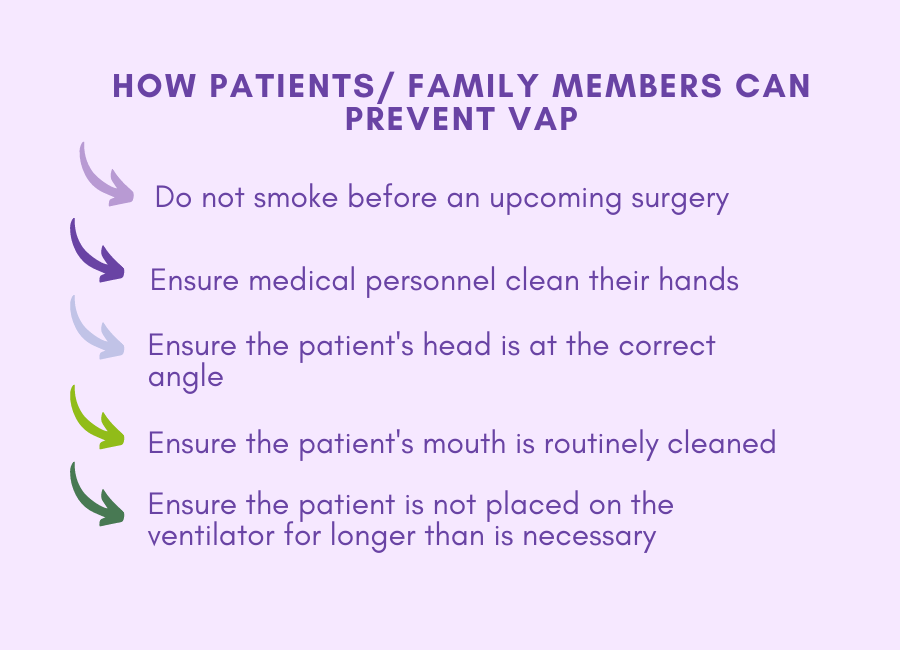
A VAP is essentially a lung infection that manifests in patients who require a ventilator to breathe. The tube that is connected to their nose, mouth or neck then feeds oxygen to their lungs. An infection occurs when germs enter this tube and gain access to the patient’s lungs.
Patient’s could require a ventilator for a multitude of reasons; the underlying fact is that most of these patients are highly vulnerable. As a result, VAPs pose a serious threat.
If you are interested you can access an informative and in-depth paper about HAI, click here.
According to the WHO “Every day, HAI result in prolonged hospital stays, long-term disability, increased resistance of microorganisms to antimicrobials, massive additional costs for health systems, high costs for patients and their family, and unnecessary deaths”.
That is why, at DrTemp, we will continue our dedication to help prevent cross- contamination and bolster infection control. We hope that the information above is educational and beneficial to your outlook on sanitary practices.









DrTemp (Pty) Ltd supplies medical devices, specializing in infection prevention and control. We are the exclusive distributor of TraxIt and NexTemp disposable clinical thermometers in Sub-Saharan Africa.
DrTemp also manufactures the O Clamp umbilical cord clamps, proudly made in South Africa.

South African Medical Device Industry Association (SAMED)
South African Health Products Regulatory Authority (SAHPRA)
Copyright © 2022 DRTEMP. All rights reserved. Website Designed and Developed by Vital Dev (Pty) Ltd.